Avoiding Posterior Calcaneal Spur

Overview
Approximately 10 per cent of the population may have heel spurs without any heel pain. Whilst recent research has raised the question of whether or not heel spurs are the result of the body trying to increase its base of support, heel spurs are still considered to be the result from strain on the muscles of the foot (in particular the plantar fascia). This may result from a biomechanical imbalance, such as over pronation.
Causes
Heel spurs develop as an abnormal growth in the heel bone due to calcium deposits that form when the plantar fascia pulls away from the heel. This stretching of the plantar fascia is usually the result of over-pronation (flat feet), but people with unusually high arches (pes cavus) can also develop heel spurs. Women have a significantly higher incidence of heel spurs due to the types of footwear often worn on a regular basis.

Symptoms
Although it may take years to become a problem, once it appears, it may cause considerable suffering. Because of proximity to the tendons, the spur is a source of continuous painful aching. The sensation has been described as "a toothache in the foot." When you place your weight on the heel, the pain can be sufficient to immobilize you.
Diagnosis
Sharp pain localized to the heel may be all a doctor needs to understand in order to diagnose the presence of heel spurs. However, you may also be sent to a radiologist for X-rays to confirm the presence of heel spurs.
Non Surgical Treatment
Rest your foot. Reduce the amount of weight-bearing activities you participate in. Get off of your feet and elevate them. This will allow healing to begin. Apply ice to your foot. Applications of ice packs that provide a comfortable cooling to the heel and arch (not a freezing cold) will help reduce pain, swelling, and inflammation. Apply the ice to the heel and arch (not the toes). Make sure it is comfortable, and leave on your foot for about 20 minutes, 3 times a day. If you have any medical problems such as diabetes, poor circulation, etc., discuss the use of ice with your doctor before applying the ice. Active Wrap allows you to apply comfortable cold therapy to your foot without messy ice cubes. Use while on the ?go.? Do not walk with bare feet. Always protect your heels, arches, and plantar fascia with good supportive shoes. Vionic Orthotic Flip Flops For Men and Women are designed for walking comfort with built in orthotic foot beds that help reduce foot pain from heel spurs. Use in the house or on the beach.
Surgical Treatment
When chronic heel pain fails to respond to conservative treatment, surgical treatment may be necessary. Heel surgery can provide pain relief and restore mobility. The type of procedure used is based on examination and usually consists of releasing the excessive tightness of the plantar fascia, called a plantar fascia release. The procedure may also include removal of heel spurs.
Bursitis Of The Foot Infection
Bursitis is the inflammation of a bursa within the body. A bursa is a fluid-filled sac that cushions some of the major joints, allowing bones, gliding muscles, and tissues to exist together without harming each other. It aids in reducing the friction between bones and the soft tissues above it. Though there are bursae all over the body, the main ones are located in the knee, elbow, shoulder, hip, and heel. These are also the ones that are the most often injured. Still, however, when you hear the word ?bursitis?, the person is usually referring to their shoulder, but it could also refer to any of the preceding areas--such as the second most common one, the hip.
Causes
Bursitis occurs when the bursae become irritated or infected, often causing pain on movement. When infection is involved, medical intervention is necessary to fight the underlying infection and prevent it from spreading, when infection is not involved, prompt medical attention can prevent the condition from becoming worse over time.
Symptoms
Symptoms of bursitis usually occur after rest and relaxation. Upon activity there is usually more intense pain in the area of the bursa. The common areas to have a bursitis in the foot are in the bottom of the heel, behind the heel near the attachment of the Achilles Tendon as well as along the side of a bunion. A bursa may also form in multiple areas especially along the metatarsal heads, or "ball" of your foot. You may actually feel the sac like fluid when rubbing the area of pain.
Diagnosis
Like all other forms of bursitis, initially the physician will take down the history of symptoms experienced by the patient, this will be followed by a detailed physical examination which involves checking for inflammation signs like pain, redness, and warmth of the heel area. The physician might examine further by moving the ankle a little to determine the exact location of pain. Further diagnostic tests including x-ray, bone scans, and MRI scan might be suggested if required.
Non Surgical Treatment
The initial course of treatment for this problem, after the usual ice and ibuprofen/aspirin routine or course, is to change footwear, especially if the onset of the problem was coincidental with a new pair of shoes. If this fails, a small heel lift (no more than ??) in both shoes may provide enough biomechanical adjustment to relieve the stress and/or friction over the area. If there is still no improvement, complete rest from running is probably advised, along with a professional consultation.
Surgical Treatment
Surgery to remove the damaged bursa may be performed in extreme cases. If the bursitis is caused by an infection, then additional treatment is needed. Septic bursitis is caused by the presence of a pus-forming organism, usually staphylococcus aureus. This is confirmed by examining a sample of the fluid in the bursa and requires treatment with antibiotics taken by mouth, injected into a muscle or into a vein (intravenously). The bursa will also need to be drained by needle two or three times over the first week of treatment. When a patient has such a serious infection, there may be underlying causes. There could be undiscovered diabetes, or an inefficient immune system caused by human immunodeficiency virus infection (HIV).
Prevention
Do not run if you have pain. When you begin running again, avoid running fast uphill or downhill until the tendon is fully healed. Start exercising when caregivers say that it is OK. Slowly start exercise such as bicycling when caregivers say it is OK. When doing exercises that put pressure on the ankles, such as running or walking, exercise on flat, even surfaces. Avoid doing these exercises on very hard surfaces such as asphalt or concrete. Stretch before exercising. Always warm up your muscles and stretch gently before exercising. Do cool down exercises when you are finished. This will loosen your muscles and decrease stress on your heel. Wear heel protectors. Use soft foam or felt heel pads (wedges or cups) to help decrease pressure against your heel. Ask your caregiver which heel pads are the best for you. Wear well-fitting shoes. Buy running or exercise shoes that support and fit your feet well. Do not wear low-cut shoes. Talk to your caregiver or go to a special exercise footwear store to get well-fitting athletic shoes. Ask your caregiver if you should wear specially-made shoe inserts called orthotics (or-THOT-iks). Orthotics can line up your feet in your shoes to help you run, walk and exercise correctly.
Hammer Toes Explanation
 Overview
Overview
Hammer, claw, and mallet toes are toes that do not have the right shape. They may look odd or may hurt, or both. Tight shoes are the most common cause of these toe problems. A Hammer toe is a toe that bends down toward the floor at the middle toe joint. It usually happens in the second toe. This causes the middle toe joint to rise up. Hammer toes often occur with bunions. Claw toe often happens in the four smaller toes at the same time. The toes bend up at the joints where the toes and the foot meet. They bend down at both the middle joints and at the joints nearest the tip of the toes. This causes the toes to curl down toward the floor. A mallet toe often happens to the second toe, but it may happen in the other toes as well. The toe bends down at the joint closest to the tip of the toe.
Causes
More often than not, wearing shoes that do not fit a person well for too long may actually cause hammer toes. Wearing shoes that are too narrow or too tight for the person for extended periods of time may eventually take a toll on the person's feet. The same is true for women who like wearing high-heeled shoes with narrow toe boxes.
 Symptoms
Symptoms
Hammer toe is often distinguished by a toe stuck in an upside-down ?V? position, and common symptoms include corns on the top of your toe joint. Pain at the top of a bent toe when you put on your shoes. Pain when moving a toe joint. Pain on the ball of your foot under the bent toe. Corns developing on the top of the toe joint. It is advisable to seek medical advice if your feet hurt on a regular basis. It is imperative to act fast and seek the care of a podiatrist or foot surgeon. By acting quickly, you can prevent your problem from getting worse.
Diagnosis
Hammer toes may be easily detected through observation. The malformation of the person's toes begin as mild distortions, yet may worsen over time - especially if the factors causing the hammer toes are not eased or removed. If the condition is paid attention to early enough, the person's toes may not be permanently damaged and may be treated without having to receive surgical intervention. If the person's toes remain untreated for too long, however the muscles within the toes might stiffen even more and will require invasive procedures to correct the deformity.
Non Surgical Treatment
The treatment options vary with the type and severity of each hammertoe, although identifying hammertoe the deformity early in its development is important to avoid surgery. Podiatric medical attention should be sought at the first indication of pain and discomfort because, if left untreated, hammertoes tend to become rigid, making a nonsurgical treatment less of an option. Your podiatric physician will examine and X-ray the affected area and recommend a treatment plan specific to your condition.
Surgical Treatment
Surgery may be the treatment of choice if conservative approaches prove unsuccessful. Usually performed as an outpatient procedure, the specific surgery will depend on the type and extent of injury to the toe. Recovery my take several days or weeks and you may experience some redness, stiffness and swelling of the affected toe. Your physician will recommend taking it easy and to keep your foot elevated while you recover.
Hallux Valgus Symptoms And Treatment
Overview
 In medical terms, a bunion, or hallux valgus, is a bony bump that forms around the joint at the base of your big toe. This joint is one of the most important parts of your foot, bearing most of your body weight. The bony bump is caused by the head of the first metatarsal bone (the long bone) behind the big toe angling out from the foot. This causes the joint to swell, pushing the big toe in towards the adjacent toes. The result is pain on the side of your foot, arch pain, and discomfort throughout the adjacent toes as well.
In medical terms, a bunion, or hallux valgus, is a bony bump that forms around the joint at the base of your big toe. This joint is one of the most important parts of your foot, bearing most of your body weight. The bony bump is caused by the head of the first metatarsal bone (the long bone) behind the big toe angling out from the foot. This causes the joint to swell, pushing the big toe in towards the adjacent toes. The result is pain on the side of your foot, arch pain, and discomfort throughout the adjacent toes as well.
Causes
Hereditary and shoe gear are probably the most likely causes. Tight pointy shoes (and high heels) may promote the formation of a bunion. A bunion may develop rapidly or develop slowly over time. Some people have bunions in their teens while others only develop a bunion later in life. Bunions come in a variety of sizes - from small to severe. In some cases, the big toe may push against the second toe, and may result in pain and a hammer toe, or progress onto a severe disfiguring foot deformity. Depending on your overall health, symptoms and severity of the bunion, the condition may be treated conservatively and/or with surgery.
Symptoms
A bony bump along the edge of the foot, at the base of the big toe (adjacent to the ball of the foot) Redness and some swelling at or near the big toe joint. Deep dull pain in the big toe joint. Dull achy pain in the big toe joint after walking or a sharp pain while walking. The big toe is overlapping the second toe, resulting in redness, calluses, or other irritations such as corns.
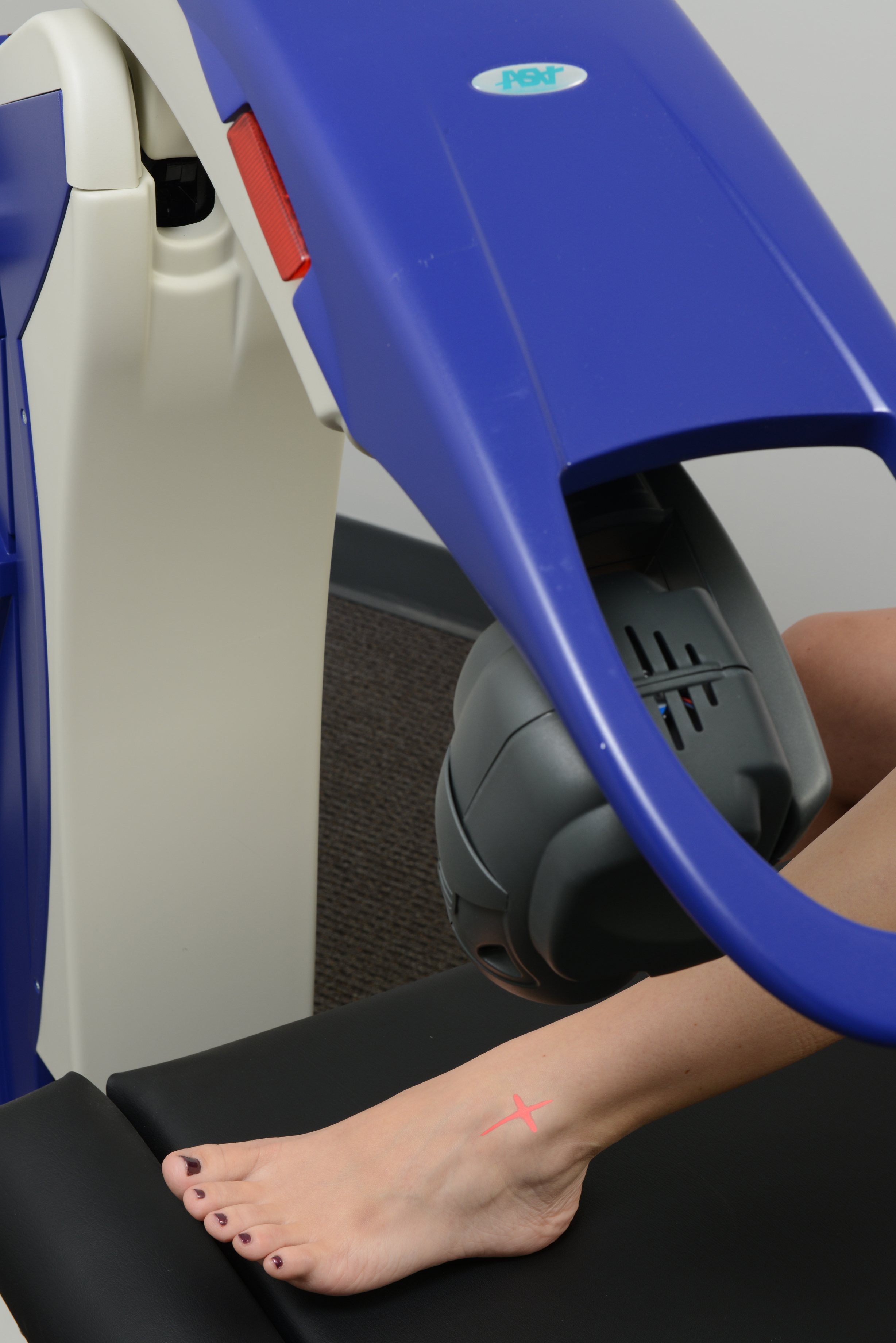
Diagnosis
People with bunions may be concerned about the changing appearance of their feet, but it is usually the pain caused by the condition that leads them to consult their doctor. The doctor will evaluate any symptoms experienced and examine the affected foot for joint enlargement, tissue swelling and/or tenderness. They will also assess any risk factors for the condition and will ask about family history. An x-ray of the foot is usually recommended so that the alignment of big toe joint can be assessed. This would also allow any other conditions that may be affecting the joint, such as arthritis, to be seen.
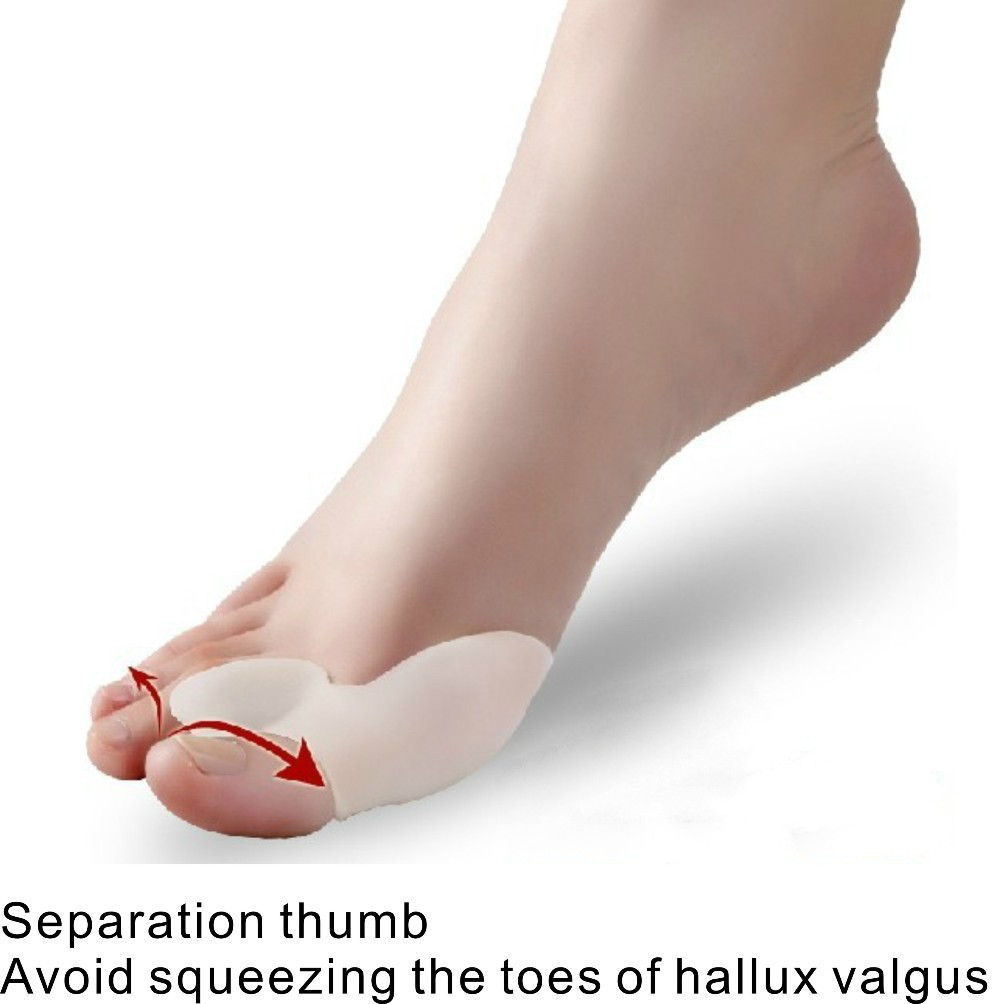
Non Surgical Treatment
This is probably the most important step. Wearing the right footwear can help reduce stress on a minor deformity and reduce the likelihood of it progressing. Recommendations are that the forefoot easily fits within the width of the shoe and there is adequate cushioning and arch support. Soft materials such as smooth leather, suede or fabric will also help to reduce irritation to the area. The podiatrist plays an invaluable role in managing patients with bunions. This is because they can offer a number of options to the patient that can help relieve pain and reduce the severity of the deformity. They can also reduce pressure on skin lesions that develop as a result of the biomechanical changes. Podiatrists can prescribe customised orthotic devices that help reduce the stress on a bunion and control biomechanical factors which cause them. These may be used in conjunction with bunion splints or cushions to further offload the area. Evidence has shown a significant reduction in pain with the use of customized orthotic devices. 
Surgical Treatment
Surgery should only be considered for bunions that are painful, not for correction of the cosmetic appearance! The primary indication for operative intervention should be pain that is not relieved by appropriate non-operative management. Although symptom-free bunions can slowly increase in size over time surgical treatment is not recommended unless significant pain symptoms develop. The prolonged recovery time associated with most bunion operations, combined with the potential for complications means that patients should be extremely cautious of undergoing bunion surgery for purely cosmetic reasons.
Overpronation Of The Feet Pain And Discomfort
When standing, pronation occurs as the foot rolls inwards and the arch of the foot flattens. Pronation is a normal part of the gait cycle which helps to provide shock absorption at the foot. The opposite movement to pronation is supination. This is also a normal part of the gait cycle just after the heel strike however over-supination is also not good.

Causes
Over-pronation may happen because the tissue that attaches to your foot bones is loose. You may be born with this problem or it may result from injuries or overuse, like from too much running.
Symptoms
Symptoms can manifest in many different ways. The associated conditions depend on the individual lifestyle of each patient. Here is a list of some of the conditions associated with Over Pronation. Hallux Abducto Valgus (bunions). Hallux Rigidus (stiff 1st toe). Arch Pain. Heel Pain (plantar fascitis). Metatarsalgia (ball of the foot pain). Ankle sprains. Shin Splints. Achilles Tendonitis. Osteochondrosis. Knee Pain. Corns & Calluses. Flat Feet. Hammer Toes.
Diagnosis
People who overpronate have flat feet or collapsed arches. You can tell whether you overpronate by wetting your feet and standing on a dry, flat surface. If your footprint looks complete, you probably overpronate. Another way to determine whether you have this condition is to simply look at your feet when you stand. If there is no arch on the innermost part of your sole, and it touches the floor, you likely overpronate. The only way to truly know for sure, however, is to be properly diagnosed by a foot and ankle specialist.

Non Surgical Treatment
The following exercises help retrain the foot and ankle complex to correct overpronation. Exercises may be performed while wearing shoes, or for an even greater challenge, in bare feet. Duck Stand. This exercise is designed to prepare for the more dynamic BT exercises ahead by waking up the gluteal muscles and teaching clients how the gluteal muscles control the degree of foot pronation. For example, when the glutes contract concentrically, they rotate the leg outward. As the leg rotates outward, the arch of the foot raises (i.e., supinates). Stand beside the BT with both heels together and feet turned outward. (Note: As you progress, perform this exercise while standing on the BT.) Try to rotate legs outward by tightening buttock muscles while tilting pelvis under. As legs rotate outward, arches of the feet raise up out of pronation. Hold position for 30 seconds. Big Toe Pushdowns. This exercise is designed to strengthen the muscle of the big toe that holds up the arch of the foot (i.e., flexor hallucis longus muscle). This stops the foot from overpronating. Stand on top of the BT dome with feet facing forward. Use gluteal muscles to raise the arches of the feet (see previous exercise - "Duck Stand"). Keep arches raised while pushing down big toe into the BT. While pushing down, tension build in the arch on the underside of their foot should be felt. Hold position for 15 seconds.
Prevention
Wearing the proper footwear plays a key role as a natural way to help pronation. Pronated feet need shoes that fit well, provide stability, contain supportive cushioning, are comfortable and allow enough room for your foot to move without causing pain or discomfort. Putting special inner heel wedges, known as orthotics, into your shoes can support a flatfoot while lowering risks of developing tendinitis, according to the American Academy of Orthopaedic Surgeons. More extensive cases may require specially fitted orthopaedic shoes that support the arches.
What Would Cause Calcaneal Apophysitis?
Sever?s disease is similar to Osgood-Schlatter disease of the knee in that they both involve a partial detachment or tearing of the tendon from the bone. The difference is location: Osgood-Schlatter occurs at the knee, and Sever?s occurs at the ankle. In Sever?s disease, which usually occurs in children from the ages of 8 to 14, the Achilles tendon begins to tear away from its insertion into the calcaneus or heel bone. This injury can be very painful and affect highly active to somewhat inactive children. Symptoms include pain that increases with activity, localized pain in the back of the foot, tenderness to the touch, and swelling. Treatment includes rest, ice, compression, elevation, and nonsteroidal anti-inflammatory medication as necessary.
Causes
The more active a child is then the greater the chance of suffering from Sever?s disease. Poor foot function such as flat feet causes the calf and Achilles to work harder and pull on the growth plate leading to Sever?s disease. Tight calves or Achilles is common in growing children and can increase tension on the growth plate.
Symptoms
The typical patient is a child between 10 and 13 years of age, complaining of pain in one or both heels with running and walking. The pain is localized to the point of the heel where the tendo-achilles inserts into the calcaneus (heel bone), and is tender to deep pressure at that site. Walking on his toes relieves the pain.
Diagnosis
Most often, a healthcare professional can diagnose Sever?s disease by taking a careful history and administering a few simple tests during the physical exam. A practitioner may squeeze the heel on either side; when this move produces pain, it may be a sign of Sever?s disease. The practitioner may also ask the child to stand on their tiptoes, because pain that occurs when standing in this position can also be an indication of Sever?s disease.
Non Surgical Treatment
When the condition flares, it is treated with activity limitation, medication to reduce inflammation (such as ibuprofen [Advil] or naproxen [Aleve]), shoe inserts, heel lifts, cold packs, and sometimes casting when it becomes especially severe. Sever condition is generally a self-limited problem that usually improves within a year.
Recovery
One of the most important things to know about Sever's disease is that, with proper care, the condition usually goes away within 2 weeks to 2 months and does not cause any problems later in life. The sooner Sever's disease is addressed, the quicker recovery is. Most kids can return to physical activity without any trouble once the pain and other symptoms go away. Although Sever's disease generally heals quickly, it can recur if long-term measures are not taken to protect the heel during a child's growing years. One of the most important is to make sure that kids wear proper shoes. Good quality, well-fitting shoes with shock-absorbent (padded) soles help to reduce pressure on the heel. The doctor may also recommend shoes with open backs, such as sandals or clogs, that do not rub on the back of the heel. Shoes that are heavy or have high heels should be avoided. Other preventive measures include continued stretching exercises and icing of the affected heel after activity.